"How do insulin sensitizing drugs work?"
- Anna Broomfield
- Aug 31, 2021
- 2 min read
If you have read my blog: "What drug therapies are available for Insulin Resistant PCOS?", you will have heard of: Metformin, Thiazolidinedione's (TZD), Sitagliptin and Byetta. This blog will explain the science behind how these insulin sensitizing drugs work.
To read my previous blog, it is available by this link.
Metformin
Metformin can move into liver cells by a transporter found in the membrane called OCT1.
Within liver cells, metformin can activate an enzyme called AMP-activated protein kinase (AMPK). This activates an intracellular protein component of the insulin receptor called Insulin Receptor Substrate 1/2 (IRS1/2), usually activated by insulin action which is impaired in resistance. This is responsible for the movement of a glucose transporter (GLUT-4) into the membrane to increase glucose uptake. This reduces circulating glucose levels which contributes to weight gain.
The image below shows a a simplified image of the effect of metformin to help visualisation.

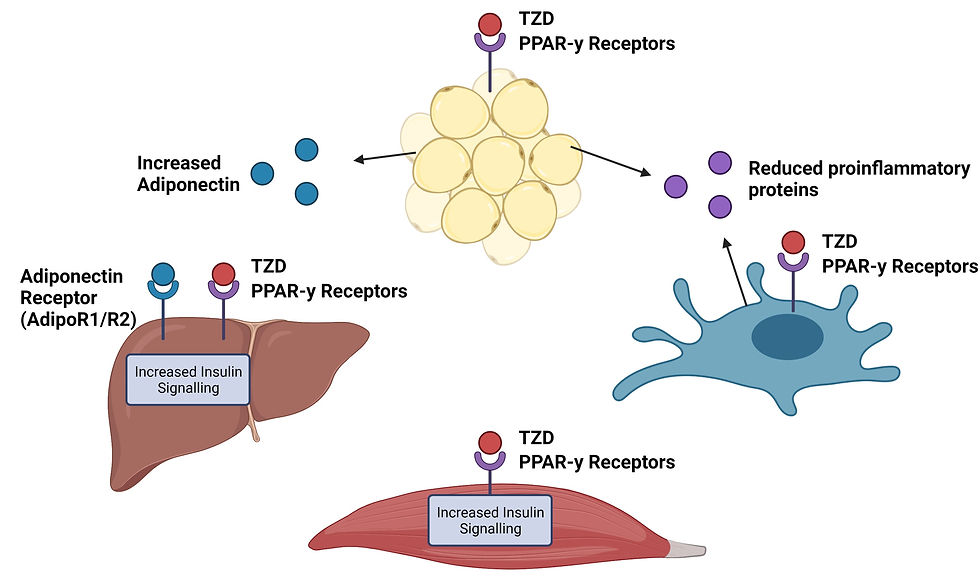
Thiazolidinedione's (TZD)
TZDs act by activating peroxisome proliferator-activated receptors (PPARs). These receptors are expressed on fat, liver, immune and muscle cells.
TZD binds to these receptors on muscle and liver cells to induce the expression of genes responsible for making proteins that cause responses to insulin. This increases insulin sensitivity and glucose uptake from the blood to prevent hyperglycaemia (too much glucose in the blood).
TZD binds to these receptors on fat cells to produce a protein called adiponectin. Adiponectin binds to liver cells to further increase insulin sensitivity and fatty acid oxidation responsible for the storage of energy.
TZD binds to these receptors on immune cells (called macrophages) to decrease the expression of inflammatory proteins called cytokines. These cytokines include: TNF-a, IL-6, resistin and MCP-1. This reduces the inflammation of blood vessels which prevents the escape of inflammatory immune cells to body cells preventing their inflammation.
The image below shows a a simplified image of the effect of TZD to help visualisation.
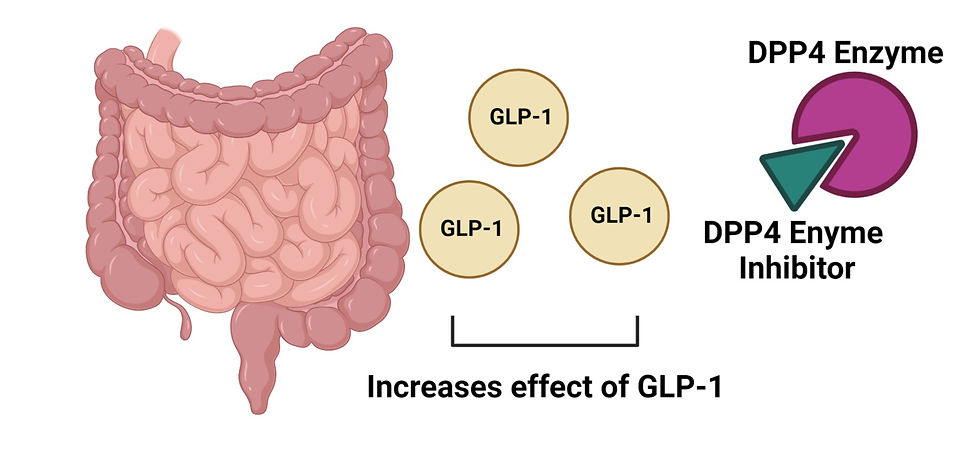
Sitagliptin (Januvia)
This drug therapy prolongs the action of incretin hormones by inhibiting the enzyme which degrades them, this enzyme is dipeptidyl peptidase-4 (DPP4). Incretins are secreted by the intestines in response to food intake to increase insulin secretion and reduce blood sugar levels. An example of an incretin includes Glucagon Like Peptide 1 (GLP-1).
The image below shows a a simplified image of the effect of Sitagliptin to help visualisation.
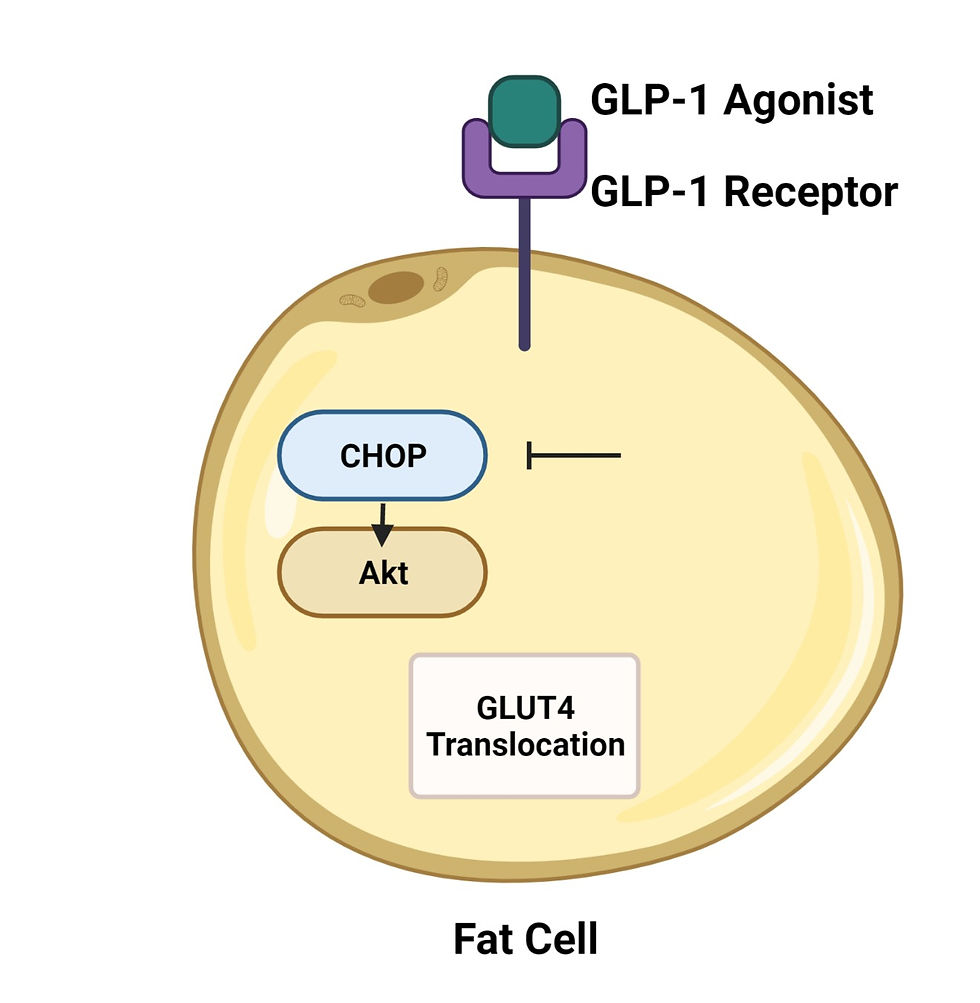
Byetta (Exenatide for injection)
Glucagon-Like Peptide 1 (GLP-1) is an important hormone mediating insulin sensitivity. Byetta works by mimicking the effect of GLP-1 to increase insulin sensitivity. This synthetic GLP-1 suppresses a cellular downstream signalling pathway called CHOP signalling.
Research has shown that blocking the protein expression of CHOP increases the expression of Akt in fat cells. This Akt protein increases the glucose transporter (GLUT4) inclusion into the membrane which removes glucose from the blood, preventing hyperglycaemia (too much glucose in the blood).


Comments